Month: January 2022
Poor anger management can lead to the use of drugs, alcohol and other addictive substances
What is anger
- Cultural groups fighting for human rights
- Nations getting together to change a system in power
- Individuals advocating for changing a law
- Communities pursuing changes for a better future


How does anger affect us
Anger can be an instantaneous reaction to an event, or a buildup of unexpressed negative emotions experienced over time and stored within us. As we experience anger, our body releases the stress hormones that during a prolonged period of time can damage our physical and mental well-being.
Anger damages our brain
Stress hormones released from anger hurt our cognitive processes such as short-term memory, decision making, and judgement. As a result, when anger is not well-managed, we act inappropriately toward others by offending, assaulting or abusing them. We might take rushed decisions and possibly use drugs or abuse alcohol to calm us down. Anger can decrease our ability to focus in situations that require clear and quick responses such as driving. Manifesting anger can become a way of living an unhealthy and destructive life.


Anger damages our heart
Anger can damage our heart in more than just a physical way by increasing our heart rate and blood pressure and causing other heart issues. It can also destroy relationships with our partners, family members, and friends and cause unnecessary issues and headaches in the work environment. Manifestation of anger in an unhealthy way can indeed have a negative impact on our children’s present and future as it creates an unsafe and threatening environment for their growth.
Talk to a healthcare professional
Often anger comes from underlying health issues. Depression, anxiety, alcohol abuse, drug use and other mental health conditions, as well as the inability to deal with everyday stresses, can make you feel irritable, overwhelmed, or even out of control. Don’t wait for things to get ugly. Take control of your anger and learn how to manage it. Get professional help and improve your life.
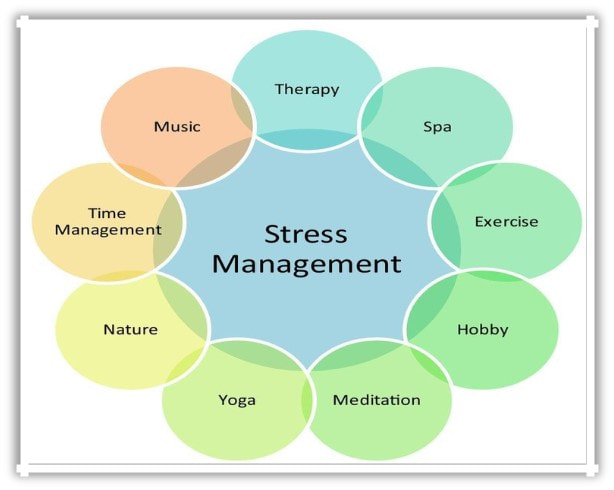
Learn ways to deal with stress
Learn breathing exercises: deep breathing relaxes our mind and lowers the heart rate.
Stress control: yoga, meditation, dance and other activities are a great way to release stress in a positive way.
Take it easy: accept the others for who they are, think like “the bigger person” when someone does things that are not done “your way” and distant yourself from the situations you can’t change or fix.
Find new hobbies: explore new thing to do and interests that make you happy, content and give you a sense of fulfillment.
Let’s look at the facts:
Our experienced professionals at the Toronto Treatment Centre can provide the right tools and coping skills to help you deal with depression and enjoy life again. We provide evidence-based treatments, including psychotherapy and other supportive services to help individuals cope with depression and improve their mental health.
Depression is a mood disorder that affects us mentally and physically: our feelings, thoughts, physical energy, coping with everyday issues, work, our environment and other people around us. With the right coping skills and support, individuals can effectively manage their depression and improve their mental health.
Signs of depression
Depression is a complex mental health condition that affects millions of people worldwide. It can manifest in various ways, and recognizing the signs of depression is crucial for early intervention and treatment. While everyone may experience depression differently, there are common signs that may indicate the presence of this condition. Understanding these signs can help individuals identify depression in themselves or others and seek appropriate support.
Persistent Sadness or Low Mood: Feeling persistently sad, down, or experiencing a general low mood that lasts for an extended period of time, typically for two weeks or more, may be a sign of depression. This may manifest as feeling hopeless, empty, or tearful, even when there is no apparent reason for the sadness.
Loss of Interest or Pleasure: Losing interest or pleasure in activities that were once enjoyable, such as hobbies, socializing, or even eating, can be a significant sign of depression. Individuals with depression may lose motivation and find it challenging to engage in activities that they once found pleasurable.
Changes in Sleep Patterns: Significant changes in sleep patterns can be an indicator of depression. This can include insomnia (difficulty falling asleep, staying asleep, or waking up too early) or hypersomnia (excessive sleepiness, sleeping for long hours). Changes in sleep patterns can disrupt the body’s natural rhythm and contribute to feelings of fatigue and lethargy.
Changes in Appetite or Weight: Significant changes in appetite or weight, either an increase or decrease, may be a sign of depression. Some individuals with depression may experience a decrease in appetite and unintentional weight loss, while others may have an increased appetite and experience weight gain. These changes can impact a person’s physical health and well-being.
Fatigue or Loss of Energy: Feeling excessively tired or lacking energy, even with adequate rest, can be a sign of depression. Individuals with depression may experience persistent fatigue, reduced stamina, and a lack of motivation to engage in daily activities.
Difficulty Concentrating or Making Decisions: Depression can affect cognitive function, leading to difficulty concentrating, making decisions, or remembering things. This can impact various areas of life, such as work, school, or personal relationships.
Irritability or Agitation: While often overlooked, irritability or agitation can be a sign of depression. Some individuals with depression may express their distress through irritability, angry outbursts, or increased agitation.
Feelings of Worthlessness or Guilt: Feeling a sense of worthlessness, guilt, or excessive self-blame can be indicative of depression. These feelings may be irrational or excessive, and individuals with depression may blame themselves for things that are not under their control or may feel worthless despite evidence to the contrary.
Withdrawal from Social Activities: Losing interest in social activities, withdrawing from social interactions, or isolating oneself can be a sign of depression. Individuals with depression may prefer to be alone or may avoid activities and relationships that were once enjoyable.
Thoughts of Death or Suicide: Persistent thoughts of death, dying, or suicide can be a serious sign of depression. Individuals with depression may express feelings of hopelessness, and the desire to end their lives may be a cry for help.
It’s important to note that not everyone with depression will experience all of these signs, and the severity and duration of symptoms can vary from person to person. However, if you or someone you know is experiencing several of these signs persistently, it may be indicative of depression, and it’s important to seek professional help from a qualified mental health professional.
Treatment for depression may include therapy, medication, lifestyle changes, and other supportive interventions. With appropriate support and intervention, individuals with depression can manage their symptoms and improve their mental health and well-being. Remember, reaching out for help is a courageous step and our team at Toronto Treatment Centre is ready to support you.
Types of depression

Depression is a mental illness that debilitates a person from normal functioning, mentally and physically, on a daily bases. Depression is a complex mental health condition that can manifest in different ways. There are several types of depression, each with its unique features and characteristics.
Major Depressive Disorder (MDD): Also known as clinical depression, major depressive disorder is the most common type of depression. It is characterized by persistent and severe depressive symptoms that interfere with an individual’s daily life. Symptoms may include persistent sadness, loss of interest in activities, changes in appetite or sleep patterns, fatigue, difficulty concentrating, feelings of worthlessness or guilt, and even thoughts of death or suicide.
Persistent Depressive Disorder (PDD): Formerly known as dysthymia, persistent depressive disorder is a chronic form of depression characterized by persistent low mood for at least two years. People with PDD may experience similar symptoms as MDD, but they may be less severe. However, the persistent nature of PDD can have a significant impact on a person’s quality of life.
Seasonal Affective Disorder (SAD): SAD is a type of depression that occurs during certain seasons, typically in the fall or winter when there is less sunlight. It is characterized by depressive symptoms that recur annually during the same time of the year and may include changes in appetite, sleep patterns, and energy levels.
Postpartum Depression (PPD): PPD is a type of depression that occurs after childbirth. It is estimated that 10-15% of new mothers experience PPD, which can manifest as mood swings, irritability, changes in appetite or sleep patterns, difficulty bonding with the baby, and feelings of guilt or worthlessness.
Bipolar Disorder: Bipolar disorder, also known as manic-depressive illness, is a mood disorder characterized by episodes of extreme mood swings between periods of depression and mania. Manic episodes may involve increased energy, impulsive behavior, elevated mood, and decreased need for sleep, while depressive episodes may involve similar symptoms as MDD.
Psychotic Depression: Psychotic depression is a type of depression that includes symptoms of severe depression along with psychotic symptoms, such as delusions or hallucinations. Individuals with psychotic depression may have difficulty distinguishing reality from delusions or may experience auditory or visual hallucinations that are related to their depressive symptoms.
It’s important to note that these types of depression are not mutually exclusive, and individuals may experience a combination of different types or subtypes of depression. Each type of depression requires a unique treatment approach, which may include therapy, medication, lifestyle changes, and other supportive interventions.
Treatments
Depression as a mental health disorder is treatable. The first step toward treatment is to contact a healthcare professional who can discuss with you the different types of treatments and help you connect with other team members. Treatments may include medication, psychotherapy, counselling, recreational therapy and nutritional therapy. Our Toronto Treatment Centre provides a safe and supportive environment for individuals to receive intensive treatment and develop coping skills to manage their depression.


Select your environment
In addition to professional help and treatment centers, it’s important for individuals with depression to reach out for support from loved ones. Social support can be a valuable coping skill, as it provides a sense of connection, understanding, and validation. Talking to trusted friends or family members about one’s feelings and experiences can help individuals feel less isolated and more supported in their journey to cope with depression.
Understanding the Risk Factors
Understanding these risk factors can help individuals and healthcare professionals identify those who may be at higher risk and take proactive steps to prevent or manage depression.
Genetic Factors: Research suggests that genetics play a role in the development of depression. If you have a family history of depression, you may be at a higher risk of developing the condition. Studies have found that individuals with a first-degree relative, such as a parent or sibling, who has experienced depression, are two to three times more likely to develop depression themselves.
Neurochemical Imbalances: Chemical imbalances in the brain, specifically involving serotonin, norepinephrine, and dopamine, have been linked to depression. These neurotransmitters play a role in regulating mood, and an imbalance in their levels can contribute to the development of depression.
Environmental Factors: Environmental factors, such as stressful life events, trauma, or a history of abuse, can increase the risk of developing depression. Chronic stress, loss of a loved one, relationship problems, financial difficulties, or work-related stress can all contribute to the onset of depression.
Personal Factors: Certain personality traits may also be risk factors for depression. For example, individuals who have low self-esteem, pessimistic thinking patterns, or a history of negative life events may be more susceptible to depression. Additionally, individuals with a history of anxiety, eating disorders, or other mental health conditions may also be at an increased risk of developing depression.
Gender: Studies have found that gender can also be a risk factor for depression. Women are about twice as likely as men to be diagnosed with depression. Hormonal changes during puberty, pregnancy, and menopause, as well as social and cultural factors, may contribute to the increased risk of depression in women.
Chronic Medical Conditions: Certain chronic medical conditions, such as diabetes, cardiovascular disease, cancer, and chronic pain, have been linked to an increased risk of developing depression. The stress and challenges of managing a chronic illness can take a toll on a person’s mental health, contributing to the development of depression.
Substance Abuse: Substance abuse, including alcohol and drug abuse, can also be a risk factor for depression. Substance abuse can disrupt brain chemistry, exacerbate depressive symptoms, and increase the risk of developing depression.
If you or someone you know is experiencing symptoms of depression, it’s crucial to seek professional help. A qualified mental health professional can provide an accurate diagnosis and develop a treatment plan tailored to the specific type of depression. With appropriate treatment and support, individuals with depression can manage their symptoms and improve their mental health and well-being.
Remember, seeking help is a sign of strength, and there is hope for recovery from depression.
Facts about marijuana use
More than 6.2 million Canadians have used weed, and many have become dependent on it. But, should you quit smoking weed? Weed products are known for their addictive properties and it is the second most used mind-altering substance in North America. Many have the impression that we can’t become addicted to weed. However, the National Institute of Drug Abuse (NIDA) considers marijuana an addictive substance that contributes to mental health disorders. Psychological dependence is very much possible in which one’s body and brain adapt to marijuana, as it changes the natural ways the brain works, negatively altering its baseline state.

What is withdrawal from marijuana like?
Withdrawal typically starts 1-2 days after you quit, and symptoms may include nausea, headaches, depressed mood, trouble sleeping, nervousness, increased anxiety, decreased appetite, and troubling dreams. The way you experience symptoms depends on how often and how much you consumed before quitting. Chronic cannabis users may also experience long-term health problems.
Having an addiction or dependence on marijuana can lead to effects even when not in withdrawal. THC can cause cognitive impairment, diminished coordination, a slower reaction time, and paranoia. The THC in weed affects dopamine, which leads to euphoria, pain modulation and anxiety. The more weed you consume, the harder it becomes to quit. Abuse of weed can make new things feel boring to you, ruining the novelties of life. Newer studies show that too much marijuana use during adolescence can cause brain long-term damage.
Addiction affects all parts of life negatively. But, quitting smoking weed on your own can be difficult, and many don’t succeed. It’s easy to get discouraged. Thankfully, there are many ways to treat this addiction and help you quit. This is facilitated with behavioural treatments and medical supervision.
Are you or someone you know struggling with an addiction to marijuana? Please contact us, we can help.
